How is Autism Treated?
There is no cure for autism spectrum disorder (ASD). Due to the unique range of needs and challenges among individuals with ASD, there is no one-size fits all treatment either.
ASD treatment often consists of a combination of therapies, interventions, and medications. ASD treatment goals include maximizing an individual’s ability to function independently and enhancing their development and learning. Early intervention and ongoing support can help individuals learn critical social, communication, and behavior skills.
What Types of Treatment are Available?
The wide range of ASD treatment options can include home-based, school-based, or clinical-based interventions. The sheer volume of treatment options can be very overwhelming to families living with ASD. Evidence-based interventions (interventions that have documented, empirical evidence of effectiveness) can lead to improved outcomes for individuals with ASD. Unfortunately not all ASD treatments have been shown to actually improve development or functioning of individuals with ASD and some treatments are potentially dangerous.
Discussion of ASD treatment options can be categorized as follows:
- Early Intervention: Early intervention has been proven effective in improving a child’s development. Early intervention is typically defined as intervention services to help children from birth to age 3 years old (36 months). Early intervention services include many of the therapies discussed below to help the child develop language, motor, and social skills such as walking and interacting with others. Early intervention services do not require a formal ASD diagnosis. Children with developmental delays or at risk of a developmental delay may request an evaluation through Missouri’s First Steps Program.
- Therapies: Depending on an individual’s needs, speech, occupational, and physical therapy may be recommended. Speech therapy can improve communication skills, occupational therapy can aid in teaching activities of daily living, and physical therapy can help individuals gain greater independence through improved mobility and balance. These therapies may be stand-alone interventions or can be incorporated into other intervention practices.
- Behavioral Interventions: Many behavioral interventions address social, communication, and behavioral challenges associated with ASD. These programs may use a combination of activities and interventions to reduce problem behaviors and teach individuals new skills. Examples of behavioral interventions include Applied Behavior Analysis (ABA); Discreet Trial Training (DTT); Early Intensive Behavioral Intervention (EIBI); Pivotal Response Training (PRT); and Verbal Response Intervention (VBI); etc. Visit the CDC’s ASD treatment page to learn more about these interventions.
- Educational Interventions: Structured educational programs with individualized behavioral interventions have been shown to improve outcomes for children with ASD. These programs utilize a combination of behavioral and therapeutic interventions to help individuals with ASD achieve educational and therapeutic goals. Examples of educational interventions include TEACCH and Early Start Denver Model. Visit Autism Speaks to read more about these interventions.
- Family Interventions: Trainings and counseling can help all family members learn skills to improve family interactions and engagement with their child(ren) with ASD. These interventions help parents and other family members manage challenging behaviors, increase social interaction and engagement, improve communication, and teach daily living skills.
- Medications: There are no medications that can cure or treat ASD. However, some medications can be used successfully to manage or mitigate some symptoms and behaviors. For example medications can be used to manage ADHD, anxiety, depression, severe behavioral problems, or seizures. The decision to begin a medication should be fully discussed with all of your providers to insure the medication is taken safely and effectively.
- Associated Medical Conditions: A number of other medical conditions frequently occur with ASD including gastrointestinal issues, difficulty sleeping, difficulty eating, seizure disorders, etc. It is important to work with providers to address these issues as well. Successful management of these conditions is likely to improve intervention outcomes.
How Do We Know Which Treatments are Safe and Effective?
Individuals with ASD, their families, and providers should select interventions that provide the best fit for the individual and are most likely to result in improved cognitive and behavior outcomes. Evidence-based practice provides a framework for families and providers to select the interventions most appropriate for the individual. The Missouri Autism Guidelines Initiative and the Autism Spectrum Disorders: Guide to Evidence-based Interventions resources are available for in-depth explanations; a summary Guide to Evidence-based Interventions is also available.
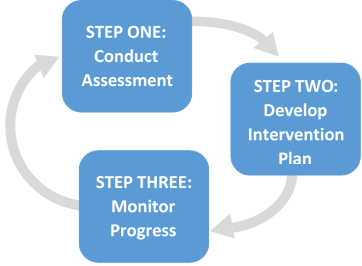
Evidence-based practice combines a professional’s expertise, evidence-based interventions, and the specific characteristics of the individual (and family) to design effective ASD interventions. To implement evidence-based practice, families and providers should engage in the intervention process. The intervention process is a three-step process consisting of conducting an assessment; developing an intervention plan; and monitoring progress.
Assessment for intervention planning identifies the unique intervention needs of each individual with ASD. A comprehensive intervention assessment should include a member(s) of an individual’s multi-disciplinary healthcare team. The assessment should include the following domains: cognitive and academic functioning; adaptive functioning; social, emotional, and behavioral functioning; and family functioning.
After the assessment, families and individuals with ASD collaborate with professionals to develop an individualized intervention plan based on the assessment results. While each individualized plan will vary, plans should include identified goals, identified and selected interventions, and identified methods for measuring progress.
As interventions are implemented, professionals and family members should monitor progress using the methods identified in the intervention plan. Data collected should demonstrate if the individual is making progress toward identified goals, if no progress is being made, or if the individual is getting worse. Based on this information, decisions can be made regarding the continuation of the specific interventions, modifying specific interventions, or discontinuing specific interventions as needed.